Project Description:
Intravenous (IV) therapy is a critical medical treatment that delivers fluids, medications,
and nutrients directly into a patient's bloodstream, typically through a catheter or needle. It is
widely employed in hospitals for various purposes, including blood transfusions and the
administration of medications. IV infiltration occurs when the fluid or medication intended for
intravenous delivery leaks into the surrounding tissue instead of being infused into the vein. This
happens when the IV catheter becomes dislodged from the vein or the vein wall is perforated,
causing the fluid to escape into the surrounding tissue. Factors such as fragile veins, rapid
infusion rates, and using a catheter that is too large for the vein contribute to infiltration. The
challenge is particularly significant in pediatric patients, especially infants and young children,
who have smaller veins that are also more fragile, and more prone to damage. Due to their
limited ability to communicate pain or discomfort, children often cannot alert healthcare
providers to issues such as infiltration, which can go unnoticed. If left untreated, IV infiltration
can cause serious complications such as tissue necrosis, infections, sepsis, and the need for
plastic surgery. The risk of these severe outcomes is heightened because current detection
methods rely on nurses checking the IV site every 1-2 hours, which can be time-consuming,
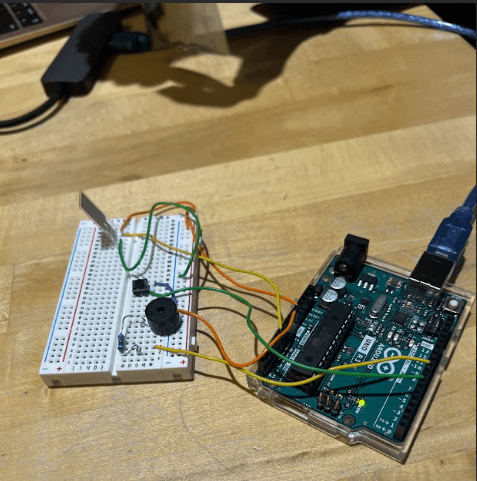
delayed, and prone to human error. To address this issue, we developed a device that
automatically and continuously monitors IV sites in pediatric patients, providing real-time alerts
when infiltration occurs. This not only protects infants and children by reducing harm, improving
comfort, and preventing complications associated with IV infiltration, but also spares families
the financial and emotional burden that often accompanies these events. Additionally, our device
reduces the manual workload for nurses in intensive care units and supports better patient
outcomes, which can contribute to improved hospital reputation and quality ratings. Our solution
utilizes a flex piezoresistive sensor that detects internal tissue deformation by converting
mechanical force—caused by swelling—into changes in analog voltage. As fluid accumulation
from IV infiltration increases pressure beneath the skin, the sensor bends slightly, resulting in a
measurable rise in voltage. Once this voltage surpasses a defined threshold, the system triggers
an audible alert via a buzzer to notify clinical staff. To evaluate the clinical relevance of our
device for monitoring IV sites, we drew inspiration from the study “Non-invasive, Multi-Modal
Sensing of Skin Stretch and Bioimpedance for Detecting Infiltration during Intravenous
Therapy” by Jambulingam et al. (2016), which demonstrated the feasibility of using non-invasive
sensing to detect infiltration-related tissue changes. Based on this framework, we conducted
preliminary testing using biological tissue models—specifically pork tenderloin and chicken
thigh—to simulate soft tissue surrounding an IV site. By placing our sensor on the tissue surface
and injecting saline to mimic infiltration, we observed clear changes in analog voltage output
from the sensor. In some cases, these changes were sufficient to trigger the buzzer alert. These
early results are promising and suggest strong potential for clinical use in pediatric and neonatal
care settings.